Table of Contents
Documentation (Clinical Loop Part-3)
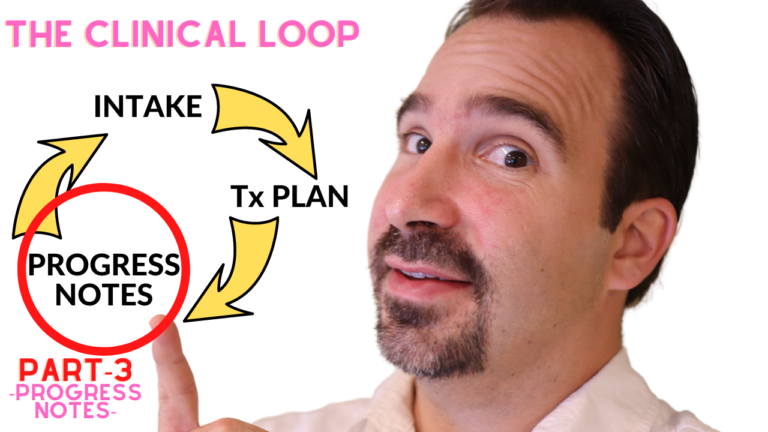
In this episode, I discuss how to write therapy progress notes and the two main methods used for documentation, SOAP and GIRP.
How To Write Therapy Progress Notes: Transcript
Hi and welcome back to the mental health Toolbox Video podcast.
My name is Patrick Martin and in this episode I’m going to show you how to write therapy progress notes as the third part of the clinical loop.
So let’s go.
Welcome.
All right, welcome back and if you’re meeting me for the first time, my name is Patrick Marten and I’m passionate about teaching people how to level up their quality of life by learning actionable coping skills.
And in this series I’m wrapping up the clinical loop.
If you missed the first two parts of this series on the Clinical Loop, you can find them at the links below:
2. How To Create A Treatment Plan
And today we’re talking about progress notes.
OK, so first things fist.
The reason this is the third part of the clinical loop and not the first or second is because we have to do the assessment first in order to gain history and knowledge of what the presenting problem is.
And then the second part is the treatment plan.
Because we need the information from the intake in order to formulate our goals and so the progress notes.
Our kind of the meat and potatoes of therapy is how we document not just the progress, but what we’re doing to do to effect change.
OK, so as you know the intervention and there are different ways we can go about documenting progress, and that’s what we’re going to cover Today.
The logistics of it, because there are different styles to it and I’m going to cover a couple of those here.
Alright, OK, so there are really two schools of thought.
SOAP VS GIRP: Two Models for Writing Therapy Progress Notes
When it comes to writing progress notes two methods, I should say, there’s the SOAP and the GIRP, and so as you can see behind me on this board, SOAP stands for subjective objective assessment and plan, whereas GIRP stands for goals, interventions, response and plan.
And we’ll talk about those and break those two down.
If you see, my daughter added a little heart there for good measure.
OK, no kid can resist a whiteboard.
You know what I mean?
OK, so let’s start with the SOAP method for progress notes.
The SOAP method is taught, oftentimes in medical school.
If you’re in the mental health field, you’ll see a lot of psychiatrists lean toward the SOAP method/acronym. A lot of MFT MSW’s. Psychologists will oftentimes incorporate the GIRP. Either one is fine. They’re just a little bit helpful framework in terms of how to navigate your progress notes, especially if you’re just starting out and you’re fresh out of college or you’re an intern as a therapist.
It’s really kind of nice to.
Try and both and see which one fits better.
Because it writing progress notes, it can feel a little mechanical at 1st and it’s not something that we just do naturally.
For example, we’re used to writing in the first person.
Whereas in Progress notes, we are encouraged to write in the third person, which can feel a little weird.
So instead of saying I, we would say “therapist or writer, or clinician did such and such and client responded.”
Or “Consumer responded this way” and so it can feel a little bit different, but it takes some getting used to.
And I’m here to help you through that, OK?
OK, so let’s start with SOAP.
The first part of the acronym there is the S, which stands for subjective.
So this is everything that the client or consumer brings to you in terms of their primary complaint, their mood, what’s going on, their stressors in their life, how they describe.
Their problem that’s the subjective portion.
OK, whereas the objective is what the clinician or practitioner observes.
This would include things.
Like
Are they oriented to time, person, place, situation?
What is their grooming like?
What is their affect like?
What is their interpersonal style or interaction like?
What is their speech like?
Are they talking fast or they talking soft?
Or they talking pressured like they?
Can’t stop talking like no matter how much you try and re redirect them they just keep talking over you.
Are they trying monopolize the conversation?
Is there something that they’re obviously not talking about that you’ve brought up and there may be avoiding a particular topic?
These are observations that you’re taking into account OK, and then the assessment that is something where you’re as a clinician trying to make an impression a clinical impression.
So this is how the person is.
Presenting and then this is what you’re noticing and so.
How can you tie that together, especially as the sessions progress and you start to develop a rapport and a history with this person, you’ll be able to kind of find those nuances about what changes in their behavior, what maybe is out of the ordinary, and even in context, right?
How they talk about someone might be different, or if you’re 18 sessions in and the client all of a sudden talks about their brother, who they’ve never brought up before, so those are things you would want to bring into your assessment.
As you’re writing your notes right in terms of their progress or things, you identify that are of clinical significance, such as target behaviors.
Clinically significant behaviors.
Compensatory behaviors.
Attachment styles.
Things of that nature.
And then the P in the SOAP model is for plan.
So the plan is of course what are you doing with this information?
How are you going to move forward?
OK, and the plan would also include things like your future interventions if you’re a psychiatrist, that’s probably going to be things like the medication regimen and things to watch for potential side effects metabolic syndrome.
Tolerance, right?
If you’re going to titrate up on a medication over time for efficacy.
Those are things that you would want to put in your plan.
If you’re a therapist, the plan might include things like target behaviors, homework, right?, mood tracking, relationship skills, grounding skills, things you’ve covered in session, and things that maybe you plan to cover if not in the next session in the coming sessions for exam.
Or I might say “OK, the 1st three sessions you know we’re going to cover mood scales, mood tracking, but then in the 4th and 5th session we’re going to cover anxiety scales and maybe the 7th and 8th session.
“We’re going to cover things like the word Journal or habituation to work on anxiety issues.”
And So what you’re showing in your progress now is your frame of mind as a clinician.
And where you anticipate taking treatment, all things considered up to that point, OK?
Alright, so now for the GIRP for progress notes.
So the GIRP acronym as I said stands for goals, interventions, response and plan.
So it’s framed a little bit differently and everybody writes there.
Now it’s in a different fashion, but I tend to prefer the GIRP model.
That’s how I was trained.
I’ve tried both, GIRP just feels more.
Natural to me.
Now.
The goal, right?
This is the thing that you are trying to address in the short term in the session, but it can also be an overarching complaint.
So if on your treatment plan, for example, the complaint was anxiety, you do want to put that into the goal right to address anxiety, but more what?
What do you plan to address in that specific session, right?
And so that’s where the goal would be to work on interpersonal effectiveness, skills, or something more specific like boundary setting and so that would be reflected then in your intervention OK.
And so then the intervention would obviously cover the basics and so this is really what the clinician is doing too.
Affect change, so First things first.
In the intervention we want to include things like assessing for risk factors, recent stressors.
And exploring client coping behaviors.
Also, if thre are recent stressors, and how they been coping and of course,
engaging the client in planning for more effective coping.
So that’s almost always going to be found under the intervention, but then you can tack on things that you are addressing specifically in that session.
For example, if your goal for this session was to work on boundary setting, then you could say things like, “writer or clinician engaged client in learning skills for boundary setting to improve quality of relationships”
Or even more specific.
“Processed with client, recent event with sister and how to avoid future arguments or verbal outbursts in response to being accused of something.”
But it’s OK to be a little specific like that, because now we’re addressing specific behaviors and problems causing the client distress, and this is also what’s known as the impairment.
So whenever we’re documenting interventions, we are really wanting to make sure that we’re speaking to the impairment, especially as far as insurance is concerned.
Because if you ever been to a documentation training, they will tell you the insurance is, especially with audits, are primarily concerned about and are paying for the intervention, not the response they’re paying for the intervention and the plan, right?
And so that’s really what you want to be able to kind of just list a couple of things about the particular problems that you’re trying to address and how you’re going about addressing them.
OK, so now for the R in the GIRP, the art in the GIRP stands for response, so the response is now what we saw in the SOAP model, which was the subjective right?
It’s kind of that piece is just reversed a little bit in the GIRP and the GIRP the response comes after the intervention.
And that speaks more to how did the client not just respond to your intervention, but this also captures that object.
If piece we see in the SOAP model.
So it kind of lumps those two together.
And the response would be things like “client presented with…, you know, as oriented times x4 and well-groomed with normal speech, linear thought process and stated mood as anxious”, right? And then you would say client discussed. you know “ABCD or 1234.”
Or you could say “client responded well to intervention, communicating understanding of boundary skills and committed to implementing skill with sister as opposed to verbal outbursts.”
And so in the response, you’re trying to paint a picture about how much clarity or how much insight the client has into the objective you’re trying to achieve or the things you discuss in session.
And of course, in the response you want to be able to touch on things like risk factors, right?
So if the client you know as you’re assessing for risk is you know what does the client respond to that does the client deny any risk issues, risk behaviors, suicidal ideations, homicidal ideations, and substance use?
Psychotic symptoms?
Or do they endorse things?
You know?
How do they respond?
Or are they not even able to engage with some of your interventions?
Do they respond to redirection?
Those are the things you want to kind of outline, and so I will often toggle between doing like a bullet-point fashion for the response.
Or sometimes I’ll do it in paragraph form.
Either is OK as long as you’re capturing kind of what’s going on there.
And we’ll talk more about that toward the end of this episode.
OK.
The Agenda.
We just covered the two acronyms for writing progress notes, but that’s only a piece of the puzzle here.
Another thing we need to consider is the agenda.
So the agenda is, you know the thing we do at the start of session.
We’re taking what we learned from the prior session or the intake.
If it’s the first therapy session.
And then we’re trying to engage the client in formulating a session agenda together, and this is to make sure that we’re getting a the best use of our time, whether it be 30 minutes, 45 minutes, 60 minutes, whatever you have planned out, basically.
Showing the client how to structure the session time responsibly, and so they also feel a commitment.
An investment in the session because oftentimes if you don’t set an agenda, the client will vent most of the session, and that’s OK.
There’s a time and a place for that.
The venting should be limited if there’s other pertinent issues, and this makes sure that you’re allowing enough room and dedicate enough time to the various concerns the client brings up or the things you observe and you agree upon addressing.
OK, so this might be like when you sit down with the client as you start session you say “OK, so you brought up these things last session.”
How much time would you like to dedicate to following up on those and where some new things that you’ve had going on during the week that you would like to address today as well?
And then oftentimes clients will bring intangible concerns as well.
Logistic things, case management needs.
And so you have to kind of plan with the client how much time and when you’re going to address those things, and it’s OK to address them in separate sessions.
But that’s part of the plan in that is in progress.
Note things you pull out of the agenda that didn’t get addressed or that need following up and homework and things like that.
And things noted in the agenda does not necessarily go into the progress.
Note this is just part of the process of spending a minute with a client at the beginning of session to see how we’re going to allocate time.
What is part of the progress now that maybe isn’t exclusive to the GIRP or SOAP model is the outline?
So by this I mean.
Over time you’ll develop a preference for how you like to outline your sessions.
I personally like to make sure that I include the numbers of sessions.
I include things like the last time I saw or talked with the client, be it face to face or via telephone call or video Tele-health session.
So what I’ll do is I’ll list that above the fold, meaning above the intervention were kind of where the goal goes.
The session number, last seen by writer and then all this goals and that will come before the intervention and then oftentimes I will frame and you know at the very bottom and the plan.
That’s where things like the homework, going into the plan.
The next time they’re going to meet with me as well as the next time they’re going to meet with their psychiatrist, right?
And so that shows whoever is looking at your notes, kind of where you know that you’re tracking treatment carefully and making sure you’re aware of any kind of follow-up appointments.
And this would include things like any ancillary supports they’re attached to or providers such as DCFS, court appointments, things like that, that just kind of show that you’re keeping your finger on the pulse of what’s going on with them and their treatment.
OK, which includes other providers right?
#3-Methods
OK, so now I would like to talk to you about three different models when it comes to writing progress notes OK?
Method-#1: Less is More
The first is the less is more model or the mentality, and it’s often times you only need to state the absolute necessary minimum amount of information in the progress note.
And that’s that, and I think the whole idea with the less is more mentality is or was that it limits the liability.
And also if a client requests their own records, oftentimes less is better because what they read may affect them adversely, OK?
Method-#2: Comprehensive Method
There’s also the other school of thought, which is the more comprehensive model, and that’s oftentimes where you include,
you know, the majority of what the person says you have quotes.
And basically.
When you’re doing a more comprehensive note, the note is more for the clinician than it is for the client in the sense that you’re writing down pertinent things that the client says that you want to follow up on right.
I personally like a little blend of the two.
You know where I I try to be succinct, but I’m also writing out kind of the different points of discussion the client brings up the different stressors, so I know in specificity what I need to follow up on not just general notions, especially if another if something should happen to me and another clinician picks up that chart, they’re able to see specifically what the client was expressing as concerns or, points of intervention for future implications.
Method-#3: The Collaborative Method
OK and then the third model, if you were, for writing progress notes, is the collaborative model and that’s more recent; that’s new.
If you’ve had any documentation training in your clinic, you will know that there’s been a lot of chatter about collaborative documentation with clients, meaning you almost actually talk about, or you do talk about, what you’re going to write in the progress.
Sometimes verbatim, sometimes in general, especially if it’s sensitive information and you might ask the client, how would you like to best phrase this?
I generally phrase this this way.
How do you feel about that?
Or is this accurate? So you’re getting a lot of clarification from the client more than permission, but clarification about how you’re going to write or how they would prefer that you phrase certain things and it actually gives the idea that the client has a lot more buy in in treatment that way and it also helps them reflect on what’s going on.
And in some cases, I know this is true in private practice, clients will be given like a summary of what was discussed.
And that’s oftentimes helpful, and so I know this is true, especially when you’re talking about things like substance use.
You want to make sure that you’re painting an accurate picture of why the client is using or when they use, such as self-medicating versus dependence issue, right?
OK, so a few other considerations I would just like to bring up.
The first of which is the location of the client or the modality.
It’s very important these days, especially in light of the pandemic, where Tele-health was kind of a taboo thing, and all of a sudden it became the main thing.
So when we’re talking about location we want to make sure that we are listing at the top of the note.
Where the client is?
Is it a telephone call?
Is it a video session?
Especially because you want to be able to make sure, as they’re not always home.
You know what I mean?
You want to make sure that you know where they are, like if they’re not at home, or if they’re in their car.
What’s the General cross street?
And the reason this is important is in case there’s an emergency, you need to be able to know where to send help.
OK, so very important, or if they’re in crisis, right? or suicidal or homicidal?
It’s really important to understand the location.
And believe me, you don’t want this to be an afterthought.
It’s not a fun lesson, OK.
Another thing to consider.
Is that anybody who picks up the client chart or reads the client chart, electronic health record, should be able to know what you’ve done, what’s worked, what hasn’t worked, and where you were going with treatment.
So there.
Should be very few bumps along the road of transition.
If the case is being handed off to someone else.
OK, so try and keep that in mind when you’re writing your notes that you just want to be able to paint a succinct picture of what’s going on so that the client doesn’t feel like they have to start all over again.
And the clinician who picks it up feels empowered.
As far as where they start their intervention.
OK, OK, and another consideration is psychotherapy notes versus progress notes.
The difference being progress notes are part of the clinical record, right, and are subject to being requested by the client or and, or subpoenaed by the court where psychotherapy notes are considered to be private notes.
If you were to keep your own psychotherapy notes separate from the chart.
Those are not subject to being subpoenaed, and so you can of course want to keep those under lock and key as well, per the law.
But just that distinction, it’s important to understand the difference.
I don’t know that it’s common practice for therapists to keep separate psychotherapy notes, but it is within your right.
OK, another consideration is mistakes.
So errors and appending.
So depending on what your platform is, if you’re just doing paper notes, or if you’re doing electronic health records.
When it comes to.
Error correcting.
There’s generally a process depending on situation, so if you’re working for an agency, there is most certainly a process for error correction, and you may not be able or have privilege to correct.
So if you see a mistake, there’s most likely a process for reporting that so they can either delete the progress note and you can rewrite it, or they might have a way for you do to what’s called appending, and that allows you to make a notation on the existing note.
If there’s a correction to be made.
OK, this is also good.
If a client points out that something is inaccurate, it allows you to go in and append the information.
So this is very helpful if you’re doing paper notes, oftentimes it requires.
Putting in a line under the note and initialing if something was a typo, and then under that writing the appendment to the note.
OK, and a couple take home points.
I want you to remember.
No note is perfect, OK?
Every therapist is a work in progress and there is no such thing as a perfect note.
Doctors, psychiatrists, therapists, nurses, we all sometimes forget to include certain information or we misspell something is just human nature and is perfectly OK.
But as you read over your notes, if you find something that was inaccurate, you know, feel free to append it.
You know, as you know, is the policy or by the correct policy of your agency.
Or if you’re a sole practitioner, you know making the do effort to append something.
If you see that it’s not correct.
Understand that you know it’s the big picture, right?
Progress notes are just about tracking treatment and making sure that we’re keeping ourselves accountable and doing the client best service that we can OK?
And one last thing when it comes to progress, notes is lag time, so especially if you’re working for an agency, you want to make sure that you get those notes in as quickly as possible, and any therapist or practitioner will tell you.
This is the most one of the most difficult things about being a service provider.
Is keeping up with your documentation.
There’s almost no worse feeling, than having you know, days or weeks of things piling up on you, and so when it comes to your systems, finding out what’s the most effective way to get your notes in on time and ideally right after the session.
It’s a personal journey and you’ll find your own way, but there are certainly different methods for going about that.
Some people prefer to wait until the end of the day and just carve out and protect an hour or two of time to just chart everything for the day at once.
Some clinicians prefer to do it each session and just stay on top of it as you go.
So whatever your method is, the most important thing is to make sure that you try and get your notes done the same day. When possible.
There will be times when you can’t get it done exactly the same day, but do make an effort to not let more than 24 hours or one working day go by where you have notes piling up.
Especially because accuracy suffers, and you actually spend a lot more time trying to remember what you discussed as opposed to just doing it while it’s fresh in your head.
And so, my recommendation is to do it immediately, but there are different ways of going about that.
Different strokes, different folk.
Yes.
And you’ll find your way.
If you have any concerns, questions or comments, please do let me know if there’s anything more about this subject you would like me to touch on, please let me know in the comments and feel free to reach out via the contact form.
And if you missed the first 2 episodes of this series, you can check those out up here and then or in the description below.
Alright, thank you so much until next time, keep thriving and make good things happen.
Bye bye now.
Want to learn more? Check out my top picks for books on self-improvement and recovery HERE!
NEED CRISIS HELP? If you need immediate crisis help with your depression, you can call the National Suicide Prevention Lifeline at 1-800-273-8255 or text “START” to 741-741
OUTSIDE THE UNITED STATES: See International Suicide Hotlines
WHERE TO FIND MENTAL HEALTH HELP:
-NAMI Referral Helpline: 1-800-950-6264
-California’s Statewide Mental Health Helpline: 1-855-845-7415
admin
Latest posts by admin (see all)
- How to Build a Referral Engine Without the “Hustle”: - January 12, 2026
- ADHD Tips for Therapists | with Dr. Jennifer Dall - May 28, 2025
- Why Therapy Fails Men (And How to Fix It) – Insights with Marc Azoulay - May 11, 2025